In the pathological structure of the musculoskeletal system, osteoarthritis occupies a leading position - about 70% of cases belong to this group. A similar problem is most common in people after the age of 50, but early signs of the disease appear even in young people. This disease has serious medical and social significance, as in many cases it becomes the cause of functional decline in working age.
Many people know about such a disease as osteoarthritis, but not all patients understand why it develops, how it manifests and what needs to be done to combat this disease. And increased awareness and caution can prevent the occurrence and progression of adverse changes.
The reasons
Osteoarthritis is characterized by the development of degenerative-dystrophic processes in all articular tissues: cartilage, subchondral bone, ligaments, muscles and tendons. The disease is considered one of the "companions of aging" because it often affects older patients. But age is not the only cause of joint deformity. The origin of the disease is quite heterogeneous and is caused by various external and internal diseases affecting the body.
For each patient, there are certain risk factors that contribute to the development of arthropathy. Therefore, the cause of joint disease combines the following conditions:
- Work hard.
- Inactive.
- Traumatic injuries.
- Joint dysplasia.
- Inflammation (arthritis).
- Overweight.
- Estrogen deficiency during menopause.
- Thyroid diseases.
- Consequences of activities on joints.
- Genetic.
As you can see, the development of arthropathy is mediated by heterogeneous factors that are, in most cases, of a mechanical or exchangeable nature. In this case, the patient's lifestyle and his profession are of no small importance, since porters, manual workers and athletes often suffer from arthrosis.
The causes of joint diseases are quite diverse, they are characterized by a local effect on the joints and a general effect on the body.
Development Mechanism
The normal function of the joint is ensured by the harmonious functioning of all its structures. But the main component of any joint is cartilage. It provides impact absorption function and resists pressure on joints. Cartilage tissue consists of cells (chondrocytes) and a substrate, the main substances of which are proteoglycan and collagen.
If the load on the joint exceeds the permissible level, then first of all there are structural disorders in the cartilage. The proteoglycans hold the lost collagen fibers, increasing the tissue's sensitivity to external influences. Destruction begins to dominate over synthesis. This is facilitated by a decrease in the nutritional properties of the cartilage when the synovial fluid contains insufficient amounts of nutrients. The imbalance of tissue renewal is supported by inflammatory responses and hormonal disturbances.
All this leads to thinning of the cartilage, which becomes rough and loses its elasticity. Due to the growth of the underlying bone tissue, the joint space is narrowed and osteoblasts - marginal growths are formed. The synovial membrane thickens, the ligaments thicken and shorten, the function of the muscles is impaired.
Pathological processes in the joints develop gradually, but do not pass without a trace. Disturbances in cartilage and other structures certainly influence the clinical picture of osteoarthritis.
Classify
Arthritis, like other diseases, has certain varieties. This must be taken into account in the clinical classification of the disease. Pathology is primary when it develops in healthy joints, or secondary if it occurs against the background of other diseases. In cases where the cause cannot be determined, they refer to idiopathic degenerative joint disease. Depending on the number of joints involved, the following varieties are distinguished:
- Single-cell disease.
- Oligoarthrosis - no more than 2 joints are affected.
- Polyarthrosis - involving from 3 groups of joints.
If the pathological process is of a general nature, then we can talk about the defeat of almost all joints of the body, including the spine, where spondylolisthesis is observed. In this case, the disease may progress to a nodular or nodular form.
It is important to understand what processes occur in the joint and to fully appreciate their severity. Therefore, be sure to take into account the stage of osteoarthritis. It is independent of the cause and is determined by pathological changes in the joint tissues:
- Stage 1 - synovitis, loss of load-bearing capacity of cartilage.
- Stage 2 - destruction of cartilage tissue, bone growth, pocket dystrophy.
- Stage 3 - bone deformity, spasticity, joint instability.
The presence of inflammatory markers should also be reflected in the classification. Therefore, osteoarthritis is distinguished with and without bursitis. In addition, the functional state of the joint is important, which is determined by the degree of deterioration:
- 1 degree - temporary limit of the function.
- Level 2 - disability.
- 3 degrees - not self-service.
All of these features should be reflected in the diagnosis of osteoarthritis, as they are important for subsequent therapy.
Symptom

Among the rheumatic diseases, the symptoms of arthropathy are quite specific. They develop gradually, but progress steadily, leading to limited physical activity. Therefore, it is especially important to suspect the disease in time so that its development can be prevented, as well as preventing complications.
When contacting a doctor, first analyze the patient's complaints. And most people worry about the pain in the joints. But with joint disease, unlike other pathologies, such as arthritis, they have the following characteristics:
- Mechanical - occurs against the background of the load and decreases at rest.
- Initiation - the appearance of pain is associated with the onset of movement (walking).
- "Mice" - periodic sharp pain with blockade of the joint, caused by the invasion of the synovial membrane between the cartilage surfaces.
At first, the person may experience only vague discomfort in the joints, accompanied by a feeling of fatigue. But over time, it develops into pain. And if at first it worries after loading, then in the future - during movement and in advanced cases it becomes constant, remaining even at rest and at night.
In addition to pain, the patient also has other symptoms of joint disease. They are both subjective and objective in nature, including the following characteristics:
- Morning stiffness for no more than 30 minutes.
- A crunching sensation (crepitus) when moving.
- Deformation of the pericellular region.
- Limited mobility.
With arthropathy of the hands, during examination, one can notice characteristic formations in the area of proximal and distal phalanges - Bouchard and Heberden nodules. The affected joints are often felt to be painful. If spasticity is formed, then there is fixation of some parts of the limbs more often than in the flexed position.
The pronounced nature of degenerative joint disease leads to a significant reduction in the patient's level of physical activity, which in turn reduces their quality of life.
Diagnose
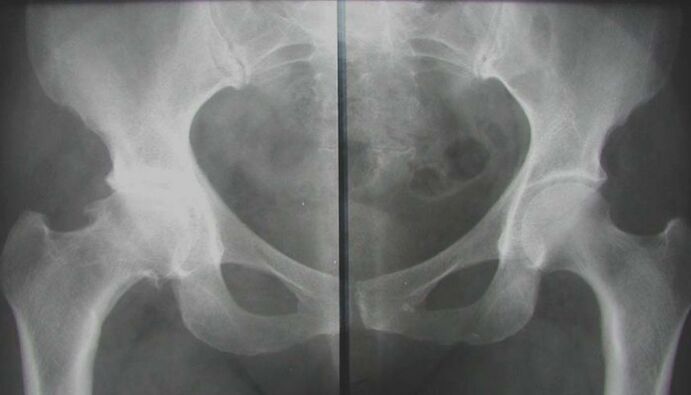
To understand why the clinical picture develops, it is necessary to confirm the pathology of the joint. This can be done by conducting the necessary diagnostic testing, including instrumental and laboratory methods. They first try to see structural changes in the affected areas, to assess their severity and prevalence. It is also necessary to identify metabolic disorders in the body, which have become a favorable background for the emergence of joint diseases. Therefore, the survey complex includes the following activities:
- X-ray.
- Magnetic resonance imaging.
- Ultrasound procedure.
- Arthroscopy.
- Biochemical blood tests (hormonal spectrum, inflammatory markers, calcium metabolism, rheumatic tests).
After the examination, you will have to consult with a trauma specialist - orthopedic trauma, to help form the correct treatment strategy for each patient.
The treatment

Comprehensive treatment of osteoarthritis is essential. This means that all available therapeutic agents are used to alleviate the patient's condition. But you need to understand that their effectiveness directly depends on the duration of treatment. With advanced forms of the disease, conservative measures will help little. Visible and lasting results can be achieved with early treatment. To treat osteoarthritis, the following methods are used:
- Medical therapy.
- Physical therapy.
- Physical therapy.
- Massage.
- Work.
Which funds are suitable for a particular patient, the doctor decides. The choice is made on the basis of the test results and the individual characteristics of the organism.
The best therapeutic effect can be achieved if correction is initiated in the early stages of the disease, when the first symptoms are just beginning to appear.
General recommendations
Since the development of degenerative changes in the joint is mediated by an increased load, it is first necessary to reduce the mechanical impact on the cartilage tissue. To do this, you should stop doing heavy, high-intensity sports. To remove the joint, any method is suitable - from walking with a cane to special immobilizers. But it is not possible to completely give up the movements and physical activities, so the dose should be taken. Walking for short distances, swimming is very helpful.
Proper nutrition plays an important role in correcting joint changes. The diet helps to improve the condition of the cartilage, but is also the main component of the fight against excess weight. Patients are advised to consume lean meat and poultry, fish, cereals; you need to enrich your diet with fresh vegetables and fruits, herbs. But in return, you should limit smoked, spicy, fatty foods, sauces and pickles. You better pay attention to foods rich in collagen, elastin and gelatin fibers: jelly meat, minced meat, dishes containing aspic, fruit jellies.
Medical therapy

Traditional osteoarthritis treatment begins with medication. Using various drugs, it is possible to eliminate not only the symptoms of the disease, but also influence the mechanism of development of the disease. This is especially important in chronic degenerative joint disease, where structural altering effects on cartilage tissue are needed. The following medications are generally recommended:
- Non-steroidal anti-inflammatory.
- Chondroprotectors.
- Blood vessel.
- Vitamins and antioxidants.
- Metabolic (estrogen, thyroid hormone).
With severe pain in joint disease, intra-articular injections of glucocorticosteroids can be performed. But such treatment should only be short-term, because with prolonged use, hormonal drugs have the opposite effect - they provoke the process of dystrophy. Systemic treatment should be combined with topical medications.
Taking medications for osteoarthritis is done as recommended by your doctor and under your doctor's control. Independent use of any drug is not allowed.
Physical therapy

Methods of physical impact help to eliminate acute signs of joint pathology. Together with drugs, they can reduce the severity of pain and inflammation, and stimulate biochemical processes in cartilage. In the complex treatment of joint diseases, the following procedures are used:
- Electrophoresis.
- Ultrasound treatment.
- wave therapy.
- Magnetic therapy.
- laser treatment.
- Mud and hydrotherapy.
Such methods affect not only the joint but also the surrounding tissues. This contributes to the activation of blood circulation, improves nutritional processes and weakens muscle contraction. Many elements of spa therapy work to improve general well-being. But at the same time, the contraindications to physiotherapy should not be forgotten: infectious diseases, tumors, cardiovascular pathologies, renal failure, bleeding, serious condition of the patient.
Physical therapy
An important aspect of non-pharmacological treatment of osteoarthritis is exercise therapy. It is known that the metabolism of cartilage tissue is clearly dependent on mechanical factors. But his strength must be matched. Only then will growth processes prevail over destruction. Therefore, gymnastics is indicated for all patients with joint diseases. But for each person, their own set of exercises is developed - taking into account the location and severity of the injury, as well as the general condition of the body.
During class hours, pain should not appear. Exercises are performed at a slow pace and only after acute symptoms have been eliminated. Avoid sudden and high amplitude movements that can cause discomfort. Physical education should be carried out under the supervision of a doctor, and after acquiring the necessary skills, you can begin exercises at home.
Gymnastics is an indispensable component in the correction of degenerative-dystrophic processes in the joints. Only regular classes have positive results.
Massage

To improve the condition of the musculoskeletal system, massage sessions are indicated. Manual action on the joints allows you to relax muscle spasms, stimulate blood circulation in soft tissues and prepare for active exercises (before therapeutic exercises). Classical massage includes the following elements:
- Caress.
- Thickness.
- Acrobatic.
- pressure.
- Iron.
It is often associated with passive movements in the affected joints. The duration of treatment is determined by the doctor and can range from 7 to 15 sessions.
Work
If the severe stages of osteoarthritis do not allow to achieve the desired effect from conservative measures, then surgical treatment is required. Its essence is to replace the joint with an artificial joint - arthroplasty. This operation is done in an open manner and under general anesthesia. Once completed, you need to rehabilitate, starting as soon as possible. And thanks to the surgical intervention, patients can completely get rid of dry joints and return to an active life. Yes, this activity is not available to everyone.
Osteoarthritis is a common problem that requires prompt and aggressive solutions. In order not to start the disease and possibly hope for the success of conservative measures, treatment should be started as soon as possible. This will avoid exacerbations, prevent the progression of changes in the joints and restore the functional capabilities of the musculoskeletal system as much as possible. Otherwise, corrective surgery will have to be considered.
























